Are your needs represented in clinical trials?
Not always, but here's how we can make progress to meet patients where they are.
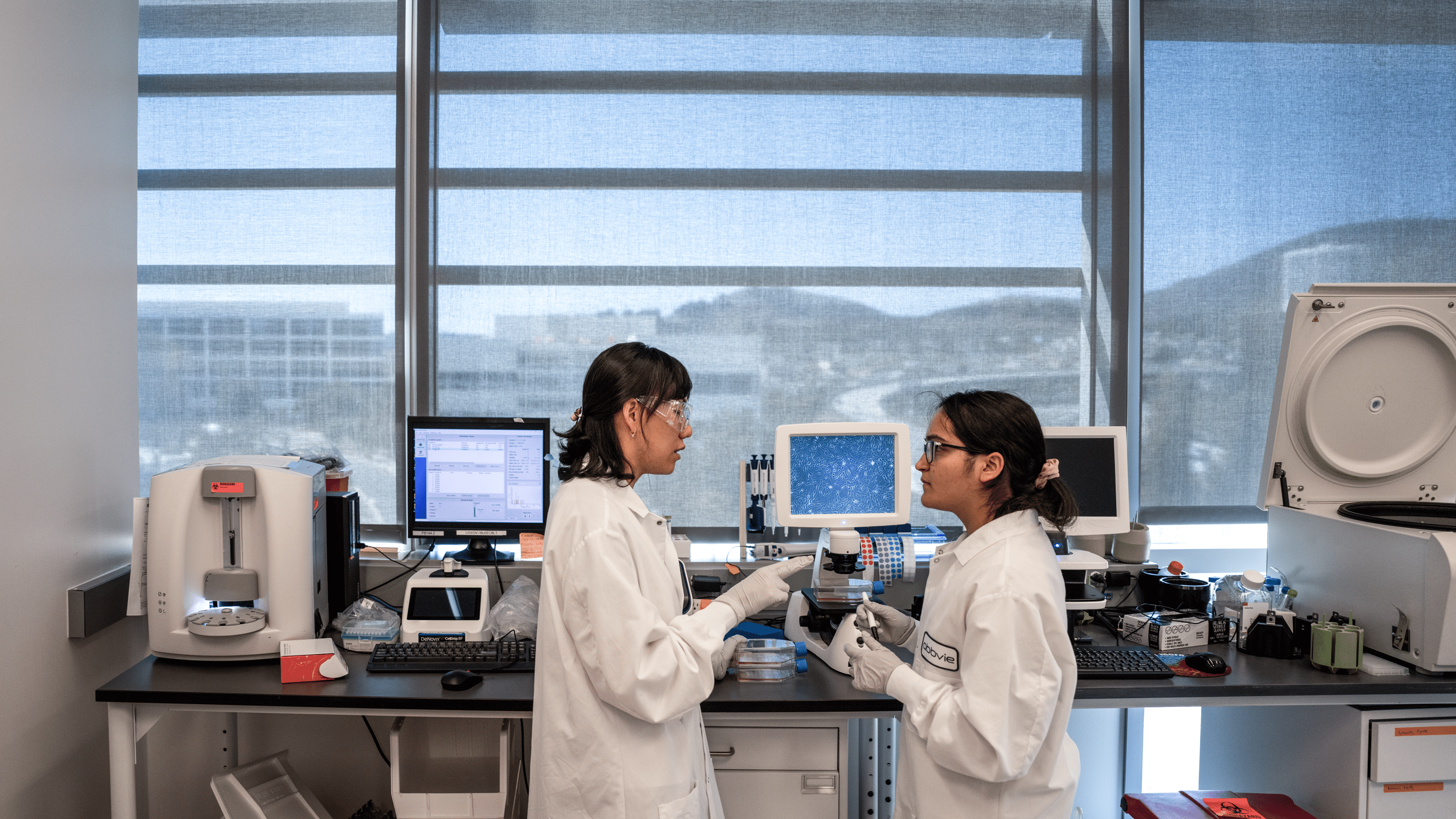
Clinical trial participation should reflect the patient population affected by the disease but in many cases representation falls short. AbbVie's head of diversity and patient inclusion looks at what needs to be done to progress future clinical research efforts.
The world relies on clinical trials to evaluate how safe and effective drugs are before they go to market. But efficacy can vary based on age, race, ethnicity, sex, or other intrinsic factors. This is why diversity matters in clinical research – yet it often isn’t seen.
The challenge is a long standing one, but recent events like the COVID pandemic, social justice movements, and the release of 2020 guidelines by the Food and Drug Administration (FDA) have shined a spotlight on the disparities that persist within clinical trials and other areas of health care.
“Seeing how the pandemic disproportionately impacted Black and Hispanic communities has really brought more attention around the health equities that are embedded across our health care system, and this is galvanizing people to make a more concerted effort to address them,” said Kim Ribeiro, head of diversity and patient inclusion at AbbVie. “For those of us within the pharmaceutical industry, this is an opportunity to revisit why this is still a problem and what we can do differently.”
Addressing resource constraints by finding ways to meet patients where they are
The time and resource constraints are among the most common barriers to patient engagement in clinical research.
“While everything else in society is pretty much on-demand, clinical trials are one of the few areas where we’re often asking the patient to come to us. For participants, this may involve taking time off work, traveling and spending long hours at the study site. That’s a hard sell for anyone, especially those who don’t have the luxury of working remotely,” Ribeiro said.
AbbVie worked to address these kinds of barriers while studying uterine fibroids in African American women. In the study, the clinical team had to collect sanitary products participants had used, every single month for over a year. To make the process easier, trial conductors offered transportation assistance, stayed open late and gave patients reminders through a mobile app. These efforts helped keep women on the trial for more than two years.
Overcoming emotional barriers and lack of awareness with education
On top of logistical barriers, emotional barriers persist when it comes to enrolling people in trials. These types of barriers may be fueled by a misunderstanding of the value of clinical trials, mistrust in the medical industry or other misperceptions.
"A lot of times when you talk to patients about considering a clinical trial, it’s very easy for them to articulate the logistical barriers, but emotional barriers are more nuanced," says Sasha Tyndale, director, patient engagement and inclusion solutions, AbbVie.
Industry groups like PhRMA say improving health literacy and education around clinical trials, particularly within underrepresented populations, can help to alleviate emotional barriers. Tyndale points out that it’s also key to align clinical trial education to where people are at in their health care experience.
“Patients are coming to the option of a clinical trial at multiple points. Some of them might be newly diagnosed. Some of them might have the disease for 10 or 15 years, and might be more experienced with managing their condition,” she said. “To be effective at educating them, we have to be able to meet them where they are.”
Broadening eligibility criteria to increase diversity in enrollment
The criteria that determine who is eligible for a clinical trial can in some cases unnecessarily exclude certain target patient populations, and according to the recent FDA guidelines, this may lead to a failure to discover important safety information about the drug under investigation.
Target populations might be unintentionally excluded when certain comorbidities are excluded or included in a trial.
“For instance, in diabetes trials on many instances, the eligibility criteria exclude people with hypertension. But hypertension is very common within the Black community and they’re also at a higher risk of having type two diabetes, so we need to think about how to balance those as we work to increase representation within our clinical trials.”
Broadening the eligibility criteria, where clinically appropriate, can ensure that clinical trial results can be generalized across the widest possible range of patient populations. This in turn would give doctors greater confidence when they’re deciding what to prescribe their patients, Ribeiro argues.
“If a doctor is considering giving a patient a drug that wasn’t tested in that patient population, you have less assurance that the data is applicable to your patient. But when we can say yes, this drug was tested on people that look like that patient you can have a bit more confidence.”
AbbVie is making progress to ensure clinical trials are diverse and inclusive; however more work is needed, as part of our broader commitment to racial justice, to reduce health disparities, address the social determinants of health and systematically enable equitable access to all our clinical research programs and medicines.
Learn more about AbbVie’s data-driven approach to clinical trial diversity.
Media inquiries:
Email: [email protected]